Activated Partial Thromboplastin Time Test – aPTT
The Activated Partial Thromboplastin Time (aPTT) Test measures how long it takes blood to clot, evaluating clotting factors and overall coagulation function. Abnormal results may indicate bleeding disorders, hemophilia, liver disease, or clotting factor deficiencies. Doctors also use this test to monitor patients on heparin therapy. Results provide essential insight into blood clotting, bleeding risk, and treatment management for safe medical care.
- $59.19
- $29.95
- Save: 49.40%
The following is a list of what is included in the item above. Click the test(s) below to view what biomarkers are measured along with an explanation of what the biomarker is measuring.
Also known as: Activated Partial Thromboplastin Time, APTT, Partial Thromboplastin Time Activated aPTT, PTT
Partial Thromboplastin
The Activated Partial Thromboplastin Time Test – aPTT test contains 1 test with 1 biomarker .
Testing Method: Photo-Optical Clot Detection
Collection Method: Blood Draw ![]()
Specimen: 2.7 mL Whole Blood 
Test Preparation: No preparation required
When is Partial Thromboplastin Time test ordered?
When a person has the following symptoms, the PTT may be ordered along with other tests, such as a PT:
- Bleeding that isn't explained or bruises that isn't easy to get rid of
- A blood clot in a vein or artery is a serious condition.
- Disseminated intravascular coagulation
- A chronic disorder that affects hemostasis, such as liver disease
A PTT can be requested in the following situations:
- When a person develops a blood clot or a woman has repeated miscarriages, as part of a lupus anticoagulant, anticardiolipin antibodies, or antiphospholipid syndrome examination
- When a person is on standard heparin therapy, the two are overlapped and both the PTT and PT are monitored until the person has stabilized. When a person is switched from heparin therapy to extended warfarin therapy, the two are combined and both the PTT and PT are monitored until the person has stabilized
- Prior to surgery, if there is a high risk of blood loss and/or if the patient has a history of bleeding, such as frequent or severe nasal bleeds and easy bruising, which could suggest the presence of a bleeding problem
What does a Partial Thromboplastin Time blood test check for?
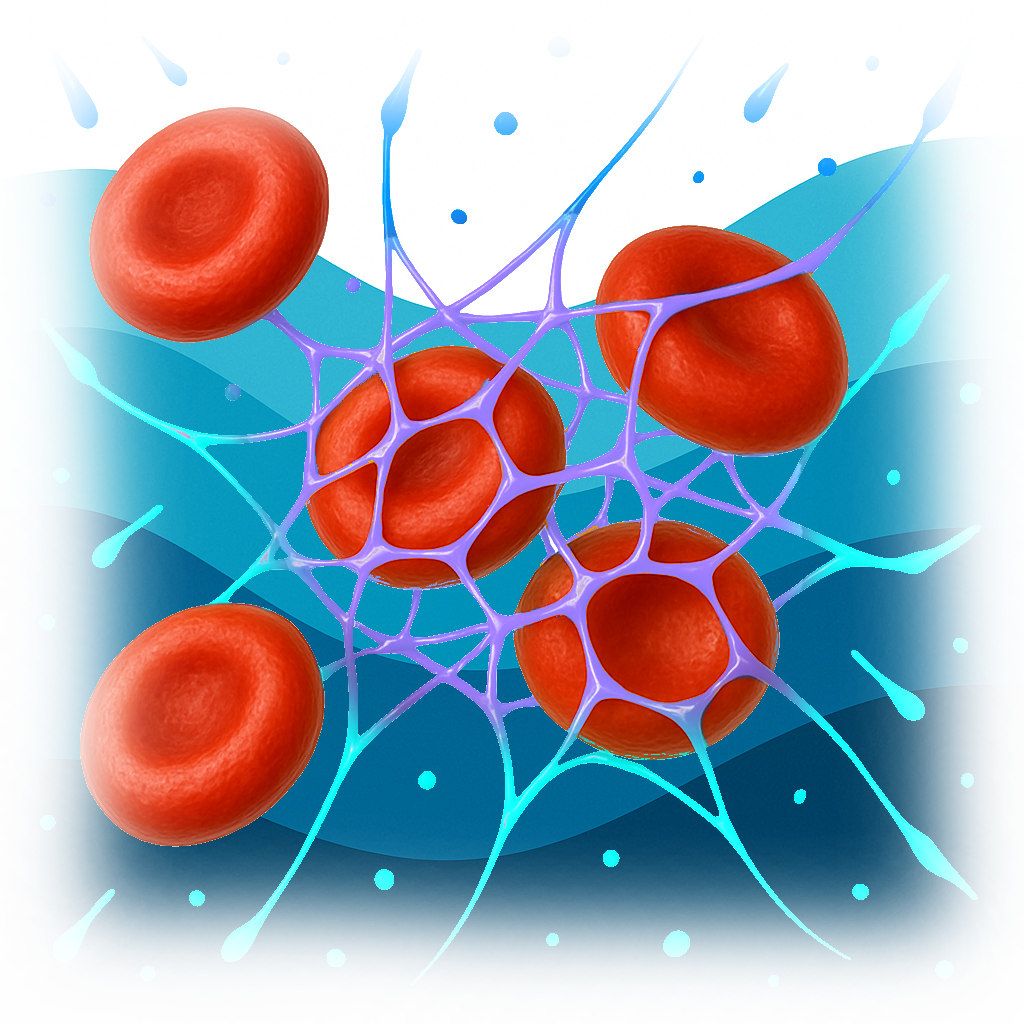 The partial thromboplastin time is a screening test that determines a person's capacity to form blood clots properly. It counts how long it takes for a clot to develop in a person's blood sample after chemicals have been administered. The PTT evaluates the number and function of specific proteins known as coagulation factors, which are crucial in blood clot formation.
The partial thromboplastin time is a screening test that determines a person's capacity to form blood clots properly. It counts how long it takes for a clot to develop in a person's blood sample after chemicals have been administered. The PTT evaluates the number and function of specific proteins known as coagulation factors, which are crucial in blood clot formation.
When bodily tissues or blood vessel walls are harmed, bleeding ensues, and hemostasis is initiated. Platelets are little cell fragments that cling to the damage site and subsequently clump together. A process known as the coagulation cascade begins at the same time, and coagulation factors are activated. Fibrin threads develop and crosslink into a net that attaches to the damage site and stabilizes it as a result of the cascade reactions. This, combined with the platelets sticking, forms a stable blood clot that seals off injuries to blood arteries, prevents further blood loss, and allows damaged areas to heal.
For appropriate blood clot formation, each component of this hemostatic mechanism must operate effectively and be present in sufficient quantities. If one or more of these factors are deficient, or if they function improperly, a stable clot may not form, and bleeding may continue.
A PTT compares a person's sample to a normal clotting time reference period. A person's PTT is considered "prolonged" if it takes longer than usual to clot. A prolonged PTT could be caused by a disease that causes one or more coagulation factors to diminish or become dysfunctional. It's also possible that it's caused by a disorder in which the body creates antibodies that attack one or more coagulation factors, impairing their activity.
A PTT may take longer than expected if the person being tested creates an autoantibody termed an antiphospholipid antibody, which interferes with the test. Because it targets phospholipids, which are employed in the PTT, this type of antibody has an effect on the test findings. Antiphospholipid antibodies can extend the PTT test result, although they are linked to increased clotting in the body. A person who makes these antibodies may be more susceptible to blood clots. A PTT could be used to assess someone who has signs and symptoms of excessive clotting or antiphospholipid syndrome.
A PTT is frequently ordered in conjunction with a prothrombin time while investigating bleeding or clotting episodes. The results of these tests will be analyzed by a health professional in order to discover the reason of bleeding or clotting episodes.
Coagulation tests like the PT and PTT are now known to be reliant on what happens artificially in the test setting and so do not always reflect what happens in the body. They can, however, be utilized to assess certain aspects of the hemostasis system. The PTT and PT tests measure coagulation components that are part of the intrinsic, extrinsic, and common chemical reaction pathways in the cascade, respectively.
Lab tests often ordered with a Partial Thromboplastin Time test:
When an aPTT test is ordered, it's often part of a broader evaluation of the clotting ability of the blood. Here are some tests commonly ordered alongside it:
-
Prothrombin Time (PT) and International Normalized Ratio (INR):
- Purpose: To evaluate the extrinsic and common pathways of the coagulation system.
- Why Is It Ordered: To provide a comprehensive assessment of the clotting system. PT/INR is particularly important for patients on warfarin therapy.
-
- Purpose: To measure the concentration of fibrinogen, a key protein in the clotting process.
- Why Is It Ordered: Abnormal fibrinogen levels can affect clotting and aPTT results.
-
Complete Blood Count (CBC), Platelet Count:
- Purpose: To evaluate overall blood health, including red and white blood cells, and platelets.
- Why Is It Ordered: To assess for conditions like thrombocytopenia (low platelet count) which can affect clotting ability.
-
- Purpose: To detect fragments of breakdown products of a blood clot.
- Why Is It Ordered: To assess for recent clot formation and breakdown, especially in the evaluation of conditions like deep vein thrombosis (DVT) or pulmonary embolism (PE).
-
- Purpose: To assess liver health.
- Why Is It Ordered: Since the liver produces many clotting factors, liver dysfunction can significantly impact coagulation tests.
-
- Purpose: To measure the activity of specific clotting factors.
- Why Is It Ordered: To diagnose specific clotting factor deficiencies, such as Hemophilia A (Factor VIII deficiency) or Hemophilia B (Factor IX deficiency).
-
Lupus Anticoagulant and Antiphospholipid Antibodies:
- Purpose: To detect antibodies associated with antiphospholipid syndrome, which can cause abnormal clotting.
- Why Is It Ordered: Prolonged aPTT can sometimes be due to the presence of these antibodies.
-
Von Willebrand Factor (vWF) Assay:
- Purpose: To measure the level and function of vWF, which is important for platelet adhesion.
- Why Is It Ordered: To diagnose von Willebrand disease, a common inherited bleeding disorder.
These tests, when ordered alongside an aPTT test, provide a comprehensive view of the body’s clotting ability and potential disorders that affect the coagulation system. They are crucial for diagnosing bleeding disorders, monitoring anticoagulant therapy, and guiding treatment for conditions that involve abnormal clotting or bleeding. The specific combination of tests will depend on the individual's symptoms, medical history, and current medications.
Conditions where a Partial Thromboplastin Time test is recommended:
The aPTT test is used to investigate and monitor various conditions, including:
- Unexplained bleeding or bruising
- Suspected bleeding disorders, such as hemophilia or von Willebrand disease
- Assessment of clotting function before surgeries
- Monitoring patients on heparin or low-molecular-weight heparin therapy
- Evaluation of patients with a history of clotting disorders or thromboembolic events
How does my health care provider use a Partial Thromboplastin Time test?
The PTT is mostly used to look into unexplained bleeding or clotting. It may be ordered in conjunction with a prothrombin time test to assess hemostasis, the body's process of forming blood clots to stop bleeding. Excessive bleeding or clotting issues are frequently investigated with these tests as a starting point.
Coagulation factors are proteins that have a role in hemostasis and the development of blood clots. When an injury occurs and bleeding begins, coagulation factors are triggered in a series of events that finally assist in the formation of a clot.
Prekallikrein and high molecular weight kininogen, as well as coagulation factors XII, XI, IX, VIII, X, V, II, and I, are all assessed using the PTT. The coagulation factors VII, X, V, II, and I are evaluated in a PT test. A health practitioner can determine what type of bleeding or clotting condition is present by combining the findings of the two tests. The PTT and PT aren't diagnostic, but they can help you figure out if you need more tests.
The following are some examples of PTT applications:
- To detect coagulation factor deficit; if the PTT is extended, additional tests can be performed to ascertain whether coagulation factors are deficient or malfunctioning, or to see if the blood contains an antibody to a coagulation factor.
- Nonspecific autoantibodies, such as lupus anticoagulant, can be detected and are linked to clotting episodes and recurrent miscarriages. As a result, PTT testing may be included in a clotting disorder panel to aid in the investigation of recurrent miscarriages or the diagnosis of antiphospholipid syndrome. The LA-sensitive PTT, a version of the PTT, could be used for this.
- Heparin is an anticoagulant medicine that is given intravenously or by injection to prevent and treat blood clots; it is used to monitor routine heparin anticoagulant therapy. PTT is extended as a result of it. Heparin must be constantly managed when it is used for medicinal purposes. If too much is given, the patient may bleed excessively; if not enough is given, the patient may continue to clot.
The PTT and PT tests are sometimes used to screen for potential bleeding tendencies before surgical or other invasive treatments based on carefully acquired patient histories.
Other tests that may be done in conjunction with a PTT or in response to aberrant results include:
- Platelet count — should be checked often during heparin therapy to detect any thrombocytopenia caused by the drug.
- Thrombin time testing – used to rule out the possibility of heparin contamination.
- Fibrinogen testing - to rule out a low level of fibrinogen as the cause of a delayed PTT.
- A second PTT test is conducted after a first PTT is delayed by mixing the person's plasma with pooled normal plasma. If the PTT time returns to normal, it indicates that one or more coagulation factors in the person's plasma are deficient. If the condition persists, it could be caused by the presence of an aberrant specific factor inhibitor or nonspecific lupus anticoagulant.
- Coagulation factor tests are used to determine how active coagulation factors are. They can identify low protein levels or proteins that aren't working properly. A coagulation factor's antigen level is occasionally tested.
- If the presence of lupus anticoagulant is suspected, a test for dilute Russell viper venom may be performed.
- Von Willebrand factor is a test that is sometimes conducted to see if von Willebrand disease is causing a prolonged PTT.
What do my Partial Thromboplastin Time test results mean?
PTT findings are usually available in seconds. A normal clotting function is usually indicated by a PTT result that falls within a laboratory's reference interval. However, a single coagulation factor deficiency may be present in low to moderate amounts. The PTT should not be extended until the factor levels have dropped to 30% to 40% of normal. Lupus anticoagulant may also be present, but it is unlikely to affect the PTT result. A more sensitive LA-sensitive PTT or a dilute Russell viper venom time can be used to test for the lupus anticoagulant if it is suspected.
A delayed PTT indicates that clotting is taking longer than usual and could be caused by a number of factors. This frequently indicates that the body's clotting ability is being harmed by a coagulation factor deficit or a particular or nonspecific antibody. Defects in coagulation factors can be acquired or inherited.
It's possible that prolonged PTT tests are caused by:
- Von Willebrand disease is the most prevalent inherited bleeding disorder, and it inhibits platelet function because von Willebrand factor levels are low.
- Hemophilia A and B are two more inherited bleeding disorders that are caused by a lack of factors VIII and IX, respectively.
- Other coagulation factors, such as factors XII and XI, are deficient.
Deficiencies in acquired factors:
- A vitamin K insufficiency. Vitamin K is required for the production of clotting factors. Vitamin K deficiency is uncommon, but it can occur as a result of a poor diet, malabsorption issues, or the use of certain antibiotics over an extended period of time, for example.
- Because the liver produces the majority of coagulation components, liver illness might result in extended PT and PTT. PT is more likely to be prolonged than PTT in patients with liver disease and vitamin K insufficiency.
- A nonspecific inhibitor, such as lupus anticoagulant—the presence of these inhibitors is usually linked to abnormal clotting, but they can also lengthen the PTT. For further information, see the individual test articles.
- Antibodies that selectively target certain coagulation factors, such as antibodies that target factor VIII, are known as specific inhibitors. They can form in people who are receiving factor replacements or they can develop spontaneously as an autoantibody in people who have a bleeding condition. Factor-specific inhibitors have the potential to induce serious bleeding.
- Heparin is an anticoagulant that will prolong a PTT if it is present in the sample as a contaminant or as part of anticoagulation therapy. The goal PTT for anticoagulant therapy is usually 1.5 to 2.5 times longer than the pretreatment level.
- The PTT is not used to monitor warfarin anticoagulation therapy, but it may be influenced by it. The PT is commonly used to track warfarin therapy.
- Anticoagulation therapy with a direct thrombin inhibitor or a direct factor Xa inhibitor are examples of other anticoagulants.
- Leukemia, severe bleeding in pregnant women prior to or after delivery, and recurrent miscarriages can all cause elevated PTT levels
The PTT results are frequently combined with the PT results to determine what ailment is present.
PTT testing may be shortened as a result of:
- Disseminated intravascular coagulation—circulating procoagulants shorten the PTT in the early phases of DIC.
- Extensive cancer
- An acute-phase reaction is a disease that causes significant tissue inflammation or trauma, which causes factor VIII levels to rise. It's frequently a one-time occurrence that isn't tracked with a PTT test. The PTT will return to normal once the condition that caused the acute phase reaction is resolved.
Most Common Questions About the Partial Thromboplastin Time, Activated (aPTT) test:
Understanding the Activated Partial Thromboplastin Time (aPTT) Test
What does the Activated Partial Thromboplastin Time (aPTT) test measure?
The aPTT test measures the time it takes for your blood to clot. It evaluates the intrinsic and common pathways of the coagulation cascade. This test is commonly used to monitor the effectiveness of treatment with heparin, a blood-thinning medication.
What do the results of the Activated Partial Thromboplastin Time (aPTT) test mean?
A normal aPTT result indicates that your blood is clotting within the expected time range, suggesting that the intrinsic and common pathways of your coagulation cascade are functioning properly. An extended aPTT can mean your blood is taking longer than normal to clot, which can be due to various conditions, including certain clotting factor deficiencies, liver disease, or the presence of anticoagulant medication in your system.
Implications of the Activated Partial Thromboplastin Time (aPTT) Test in Various Health Contexts
Why is the Activated Partial Thromboplastin Time (aPTT) test important?
The aPTT test is essential in evaluating the body's clotting pathways. It's commonly used to monitor patients receiving heparin and can assist in diagnosing clotting disorders. Prompt identification and treatment of clotting disorders can prevent severe complications, including deep vein thrombosis (DVT), pulmonary embolism (PE), and stroke.
Can the Activated Partial Thromboplastin Time (aPTT) test be used in the management of certain diseases?
Yes, this test is vital in the management of conditions that involve the blood's clotting process. For example, patients receiving heparin for clot prevention or treatment will often undergo routine aPTT tests to monitor the medication's effectiveness and adjust the dosage if necessary.
Interpreting the Results of the Activated Partial Thromboplastin Time (aPTT) Test
What does a prolonged Activated Partial Thromboplastin Time (aPTT) test result indicate?
A prolonged aPTT can indicate several conditions. These include hemophilia, von Willebrand disease, disseminated intravascular coagulation (DIC), or the effects of anticoagulant therapy like heparin.
What does a shortened Activated Partial Thromboplastin Time (aPTT) test result indicate?
A shortened aPTT is less common but could indicate an increased risk of clotting. It may occur in conditions such as disseminated intravascular coagulation (DIC), cancer, or in the initial stages of a clotting event.
Activated Partial Thromboplastin Time (aPTT) Test and Treatment Decisions
How can Activated Partial Thromboplastin Time (aPTT) test results impact treatment decisions?
The results of an aPTT test can guide treatment decisions, especially in patients taking heparin. If aPTT is too high, the heparin dose might be reduced to decrease bleeding risk. Conversely, if aPTT is too low, the heparin dose might be increased to ensure sufficient anticoagulation.
Can the Activated Partial Thromboplastin Time (aPTT) test results guide the choice of medication?
Yes, aPTT results can guide anticoagulant therapy. It is primarily used to monitor heparin treatment, although it is not used to monitor warfarin, which is monitored using the INR (international normalized ratio) test.
Considering the Patient's Context in the Activated Partial Thromboplastin Time (aPTT) Test
Can the presence of other diseases influence Activated Partial Thromboplastin Time (aPTT) test results?
Yes, liver disease, vitamin K deficiency, or other conditions that affect the clotting factors can influence the aPTT test results.
Can lifestyle changes affect the Activated Partial Thromboplastin Time (aPTT) test results?
Lifestyle changes per se do not usually affect aPTT results. However, certain medications, supplements, or foods that alter coagulation, such as high vitamin K foods or certain over-the-counter medications, can potentially affect the results.
Technological Improvements and Limitations of the Activated Partial Thromboplastin Time (aPTT) Test
What are the limitations of the Activated Partial Thromboplastin Time (aPTT) test?
The main limitation is that aPTT is sensitive to variables such as sample handling and the specific reagents used in the assay. It may also be influenced by non-specific inhibitors and certain antiphospholipid antibodies.
Can the results of the Activated Partial Thromboplastin Time (aPTT) test be influenced by technical issues?
Yes, pre-analytical errors such as inappropriate sample collection, handling, or transport, as well as incorrect ratio of blood to anticoagulant in the collection tube, can affect aPTT results.
Can the Activated Partial Thromboplastin Time (aPTT) test replace other coagulation tests?
No, the aPTT test is just one component of coagulation testing and evaluates specific parts of the coagulation pathway. Other tests, such as the Prothrombin Time (PT) and platelet count, provide different information and are often used together with aPTT for a more comprehensive view of a patient's hemostasis system.
Can the Activated Partial Thromboplastin Time (aPTT) test be combined with other lab tests?
Yes, aPTT is often performed along with other tests such as the PT/INR, fibrinogen test, and platelet count when a comprehensive evaluation of hemostasis is required.
Can the Activated Partial Thromboplastin Time (aPTT) test be used to monitor therapy with direct oral anticoagulants (DOACs)?
No, aPTT is not sensitive to the anticoagulant effects of DOACs such as apixaban or rivaroxaban.
Understanding Special Populations and the Activated Partial Thromboplastin Time (aPTT) Test
Can the Activated Partial Thromboplastin Time (aPTT) test be used in pregnant women?
Yes, aPTT can be used in pregnant women. However, it's essential to note that pregnancy can cause physiological changes that may slightly alter coagulation test results.
How is the Activated Partial Thromboplastin Time (aPTT) test used in people with lupus or lupus anticoagulant?
In people with lupus or lupus anticoagulant, aPTT can be prolonged. However, because lupus anticoagulant can paradoxically increase the risk of thrombosis, a prolonged aPTT does not correlate with a bleeding risk in these patients.
How is the Activated Partial Thromboplastin Time (aPTT) test used in people with liver disease?
In people with liver disease, aPTT can be prolonged because the liver produces many of the coagulation factors. Thus, aPTT can be used as a measure of liver synthetic function.
Future Direction and Use of the Activated Partial Thromboplastin Time (aPTT) Test
Will the Activated Partial Thromboplastin Time (aPTT) test always be necessary for heparin monitoring?
While aPTT is currently the standard for heparin monitoring, future research or technology could potentially lead to the development of more precise tests or even heparin formulations that do not require monitoring.
Can the Activated Partial Thromboplastin Time (aPTT) test be replaced by new tests in the future?
It's always possible that new tests could be developed that provide more information or are more convenient. However, as of now, aPTT remains a fundamental part of evaluating the coagulation system.
Are there potential improvements for the Activated Partial Thromboplastin Time (aPTT) test?
One area of potential improvement is standardization. While the aPTT test is broadly standardized, there can still be variations in results due to the different laboratory reagents and methods used.
Is there a role for genetics in the Activated Partial Thromboplastin Time (aPTT) test?
While there isn't a direct role for genetics in the aPTT test itself, certain inherited conditions can cause a prolonged aPTT. These include Hemophilia A and B, and von Willebrand disease.
Are there other tests being developed that work better than the Activated Partial Thromboplastin Time (aPTT) test?
While research is always ongoing, the aPTT test remains a critical part of coagulation testing. Newer tests may be able to provide more specific information or may be easier to use, but these would likely supplement, not replace, the aPTT.
How might future research impact the use of the Activated Partial Thromboplastin Time (aPTT) test?
Future research may help refine the aPTT test or guide its use in new clinical scenarios. As our understanding of coagulation improves, this may help us better interpret aPTT results.
What is the role of the Activated Partial Thromboplastin Time (aPTT) test in personalized medicine?
In the context of personalized medicine, aPTT is a critical test to ensure the safe and effective use of anticoagulant therapy, such as heparin, as it helps tailor the treatment to the individual patient's needs. By regularly monitoring aPTT, doctors can adjust the dosage to reach optimal therapeutic outcomes.
We advise having your results reviewed by a licensed medical healthcare professional for proper interpretation of your results.


